
The Minute 12 Tell:
Debugging Standing Desk Sciatica
Minute 12 is the tell. Not because your standing desk is “bad,” but because your body is quietly tallying a pattern: locked knees, shallow breathing, and a posture that turns you into a well-behaved statue—until your leg files a complaint.
Standing desk sciatica is often a flare of sciatic-nerve symptoms—pain, tingling, numbness, or weakness—aggravated by static standing, joint locking, and bracing. It’s mechanical and repeatable, which is good news: it can be debugged. If you want a quick baseline on what counts as sciatic symptoms versus “random tightness,” start with a plain-language overview of sciatica nerve pain patterns.
Stop guessing and losing focus. Don’t let your nervous system treat your desk like a threat.
The Workday Protocol
- 60-second mid-email resets
- 30-second self-tests
- Automatic “soft knee” setups
What’s Inside
- Symptom-onset timing
- Relapse prevention
- Setup tweaks (mats & footrests)
No anatomy lecture. No heroic stretching. Just the next safe step.
Locked knees turn standing into a rigid “postural statue,” often shifting load into the low back/hips and increasing tension down the sciatic pathway. Quick fix: soften knees, stack ribs over pelvis, and stand 60/40 (slight weight shift, not perfectly even). Add 10–15 seconds of tiny ankle/calf movement to restore circulation. If pain shoots below the knee, worsens, or you notice numbness/weakness, get medical guidance.
Table of Contents
Locked-knee sciatica: spot it in 15 seconds
This isn’t a personality flaw. It’s a stance. And it has a signature: you feel fine at first… then your back, hip, or leg starts sending a sharp little memo. If you’ve ever noticed it arrives after a stretch of focused work—email, spreadsheet, “just one more tab”—you’re already close to the answer. (If the same thing happens when you’re forced to stand still in public, this may feel uncomfortably familiar: how to stand in line with sciatica is basically the same problem in a different costume.)
- Check 1: Are your knees fully straight, like you’re standing at attention?
- Check 2: Are your thighs and glutes “on” even though you’re just reading?
- Check 3: Is your weight perfectly even, like you’re trying to be “correct”?
If you said yes to 2 or more, locked-knee + static standing is a strong suspect. (I learned this the hard way: I once “fixed my posture” so aggressively that my body felt like it was filing a complaint in triplicate. It wasn’t heroic. It was stiff.)

The signature feel: “fine at first… then the zing”
Many people report a delayed onset: the first few minutes are okay, then the discomfort ramps—often down the buttock, back of thigh, or into the calf. That delay matters because it points to a load-and-tension build, not a single wrong movement.
Below-knee warning: when it’s not just “tightness”
If symptoms are traveling below the knee (especially with tingling or numbness), treat it with more respect. That doesn’t mean panic—it means stop experimenting with aggressive stretches and “power poses,” and start using conservative, low-risk adjustments (and professional guidance if it’s persistent or worsening).
Curiosity gap: why it waits until minute 12
Because your nervous system is patient… until it isn’t. Static standing can quietly increase tension through calves/hips and encourage bracing through the trunk. The longer you hold the statue, the louder the message.
- Locked knees + bracing is a common combo
- Delayed “zing” suggests a build-up pattern
- Below-knee symptoms deserve extra caution
Apply in 60 seconds: Unlock your knees and do 10 seconds of tiny ankle movement right now.
Safety first: when to stop and get checked
Let’s keep this grounded: most sciatica-like symptoms improve over time, but some signals should never be “posture-hacked.” The American Academy of Orthopaedic Surgeons notes that a large share of people improve without surgery over several weeks—yet they also emphasize evaluating symptoms that suggest more serious nerve involvement. And the American Medical Association has highlighted that numbness, weakness, or bowel/bladder changes are not normal “wait it out” signs. If you want a clearer “don’t debate this” checklist, keep a bookmarked guide to low back pain emergency warning signs.
Quick disclaimer (plain English, no drama)
This article is educational, not medical advice. If anything here increases sharp, radiating pain—stop. If you’re unsure, get a clinician’s input. Your body is not a puzzle you solve by force. (Also: if you notice your mind spirals into symptom-googling at 2 a.m., you’re not alone—here’s a calm read on cyberchondria and chronic pain.)
Go now: weakness, foot drop, bowel/bladder changes
- New or worsening weakness in the leg/foot
- Foot drop (tripping, can’t lift the front of the foot well)
- New bowel or bladder changes or saddle-area numbness
- Severe, rapidly worsening pain with fever or after major trauma
Book soon: worsening pain, persistent numbness, sleep-disrupting symptoms
If symptoms are getting worse across days, interrupting sleep, or not improving with conservative changes, that’s a good time to check in. You’re not “failing at ergonomics.” You’re being smart with nerve-related symptoms.
- Yes if symptoms ramp when you stand still and ease with gentle walking
- Yes if locking knees feels “stable” but later feels worse
- No if you have red flags (weakness, foot drop, bowel/bladder changes)
Next step: If you’re a “yes,” use the 60-second reset first—then adjust your workstation so you don’t re-lock without noticing.
Who this is for / not for
Let’s do the fastest fit check on the internet. If you’re the right reader, you’ll feel seen in a slightly annoying way (the good kind).
- Your pain spikes when you stand still
- You “forget to breathe” during focus
- You feel compelled to stand perfectly straight
- Walking helps more than standing
- You have red-flag symptoms (weakness, foot drop, bowel/bladder changes)
- Your pain started after major trauma
- You can’t bear weight or symptoms are rapidly worsening
- You need a diagnosis more than a desk protocol
For you if your pain spikes when you stand still
That pattern screams “static load problem.” Not “you’re too weak.” Not “your desk is cursed.” Static load is simply a fancy way of saying: your body doesn’t love being a coat rack. If this flare pattern keeps repeating across the week, you’ll also recognize the wider picture in desk job sciatica flare-ups.
Not for you if you have red flags or recent trauma
If your nervous system is waving big flags, honor that. Ergonomics is powerful, but it’s not emergency medicine.
Curiosity gap: the “workday pattern” that changes the diagnosis
Two people can say “sciatica,” but their patterns differ: one worsens with sitting, one worsens with standing, one hates transitions. Your pattern is often more useful than a label—especially when you’re choosing what to do during the next hour of work.
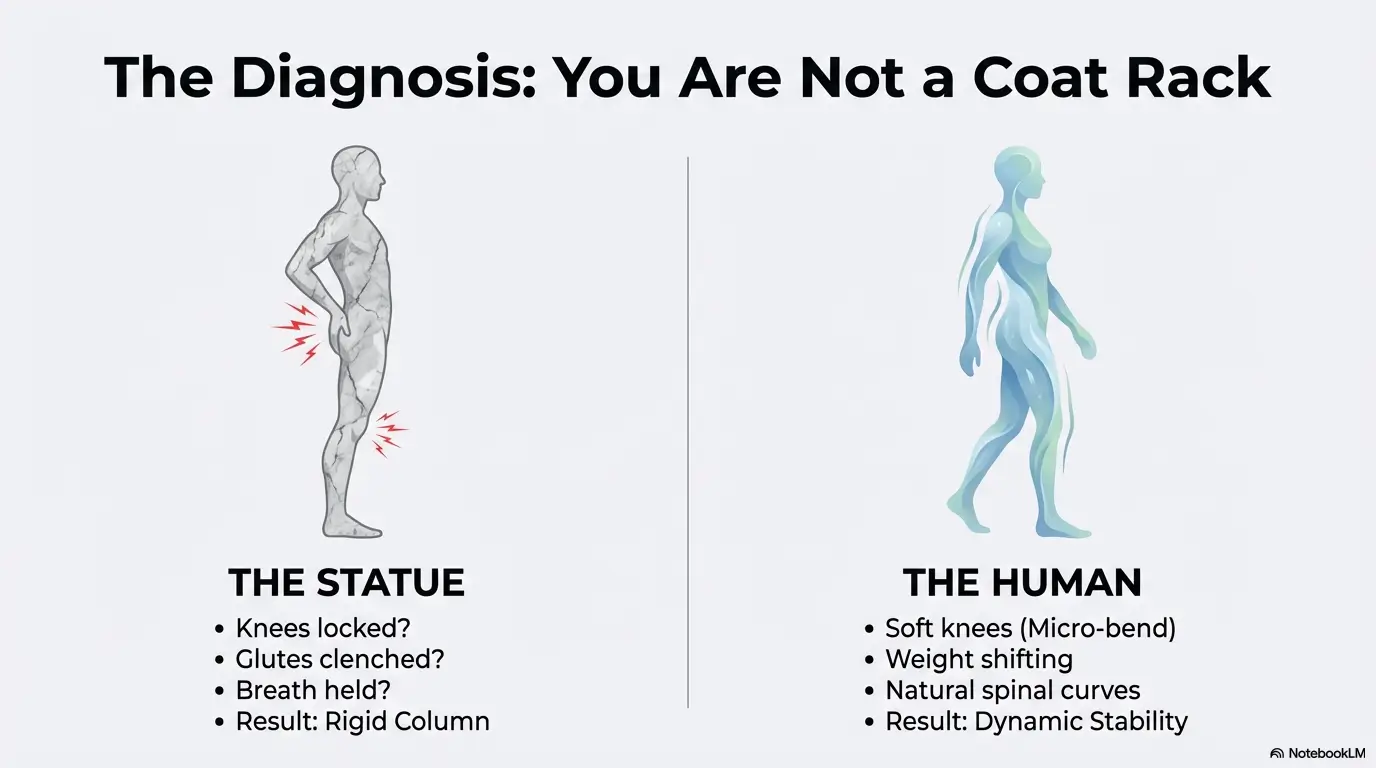
Locked knees → nerve pain: the chain reaction competitors skip
You don’t need an anatomy lecture. You need a model you can feel. Here it is:
Translation: you stand to feel better, but you accidentally become a rigid column.
The U.S. National Library of Medicine’s MedlinePlus describes sciatica as symptoms (pain, numbness, tingling, weakness) that travel along the sciatic nerve pathway. That matters here because what you’re managing at the desk is often irritation sensitivity, not a single “tight muscle.”
Calves-to-glutes tension: the hidden “pulled rope” effect
Locked knees subtly pull tension through the back line—calves, hamstrings, glutes. Your body loves stability, so it responds with more stiffness. It feels “supported” right up until it feels wrong. (Anecdote: I once stood so still during a long call that my calves felt like guitar strings. The call ended. My leg pain didn’t.)
Pelvis + ribcage stacking: why bracing travels downward
“Stand tall” often turns into “brace hard.” When the ribs flare and the pelvis tips, your trunk tries to stabilize with tension. That bracing can change how load moves through hips and legs. The fix is not collapsing. It’s stacking with breathing.
Open loop: why stretching hamstrings can backfire on flare days
If you stretch aggressively while the nerve pathway is irritated, you may feel “more pull” but less relief. On sensitive days, you want gentle motion and unloading before long holds. We’ll come back to this in the micro-break menu and FAQ.
Show me the nerdy details
Static standing increases continuous muscle activation (especially calves and postural stabilizers) and reduces natural variability in joint angles. The nervous system often prefers movement “noise” over rigid holding patterns. A small knee bend changes ankle-knee-hip alignment, reduces end-range joint locking, and makes weight shifting easier—so the system can distribute load instead of concentrating it.
Fix in 60 seconds: unlock, stack, shift (the reset protocol)
This is the part you can do mid-email without announcing, “I’m doing biomechanics now.” The goal is not perfect posture. The goal is reducing the rigid-column effect and restoring tiny movement so your system calms down.
Soften knees 1–2%. Not a squat. Just exit the end-range lock.
Ribs over pelvis. Long exhale for 4–6 seconds to de-brace.
Weight 60/40. “Tripod foot” (heel + big toe + little toe).
Tiny ankle/calf movement for 10–15 seconds. Circulation + safety signal.
If symptoms increase sharply, stop and switch to a gentler option (perch or short walk).
Step 1: “Soft knees” (not a squat)
Think “micro-bend.” Your quads shouldn’t be screaming. You’re simply telling your joints: we’re not locking down today. (Anecdote: the first time I tried this, I realized how much I was “holding my body up” like a mannequin. No wonder my back felt offended.)
Step 2: Ribs over pelvis + long exhale (de-brace)
Exhale like you’re fogging a mirror—slow, controlled. Many people unintentionally brace when they concentrate. That brace can travel down the chain.
Step 3: 60/40 weight shift + tripod feet
Perfectly even weight is overrated. A slight shift reduces static load. You can alternate which side gets the 60 every minute or two.
Step 4: 10–15 seconds ankle micro-movement (circulation signal)
Tiny movement beats heroic movement. Heel lift micro-pulses, ankle circles, or toe taps—whatever is subtle and pain-free.
Use this if you keep standing until you’re flared—then swear off standing forever.
- Input 1: Your current stand block (minutes): __
- Input 2: Your symptom onset time (minutes): __
- Input 3: Your “safe buffer” (minutes, start with 5): __
Output: New stand block = onset time − buffer. If onset is 12 and buffer is 5, your new block is 7 minutes. Then you cycle (perch/sit/walk) before you re-stand.
Neutral action: Set one timer for the next work block and run this like an experiment, not a test of willpower.
30-second self-tests: confirm your real trigger
These tests are designed to answer one question: what change reduces symptoms fastest—without guessing. Think of them as “debugging” your stance.
Test A: Toe wiggle test (are you “gripping the floor”?)
Stand in your usual stance. Try to wiggle all toes lightly for 5 seconds.
- If it feels hard, you’re likely gripping the floor and over-stabilizing.
- Fix: soften knees, shift 60/40, and let the toes relax.
Test B: Wall stack check (is your setup forcing a brace?)
Stand with your back near a wall. You don’t need to flatten your spine—just notice if your head or ribs are far forward. If you feel like you must brace to “stand up straight,” your workstation may be pulling you forward (monitor too low, keyboard too far, desk too high).
Test C: Footrest swap (does symptom intensity drop fast?)
Put one foot on a footrest (or a sturdy book) for 20 seconds. Then switch feet.
- If symptoms ease quickly, you likely benefit from hip angle variation and reduced static load.
- Fix: schedule footrest cycling (not random) and lower your “stand dose.”
Curiosity gap: the one spot you don’t feel—but drives everything
Breathing. Seriously. When you hold your breath during concentration, your trunk stiffens. When your trunk stiffens, your hips often stop moving. When hips stop moving, your legs take the stress. You don’t feel the breath-hold… you feel the consequences.
- Toe wiggle reveals over-gripping
- Wall check reveals setup-driven bracing
- Footrest swap reveals a need for angle variation
Apply in 60 seconds: Do Test C right now—20 seconds per side—and keep the change that calms symptoms.
Setup that prevents relapse: make “soft knees” effortless
If your setup demands bracing, you will brace—especially when you’re busy. OSHA’s workstation guidance emphasizes changing positions and avoiding staying in one posture too long. The quiet lesson: your workstation should support variety, not force you into one “perfect” stance. If you’re still deciding whether the real fix is “standing more” or “sitting better,” compare options in ergonomic chair vs standing desk.
Desk height: eliminate the reach → brace loop
If your desk is too high, your shoulders rise, your ribs flare, and your whole trunk tightens. If it’s too low, you hunch and load your back. Aim for a work surface that lets elbows rest comfortably near your sides while typing—without shrugging.
Monitor height: end the chin-forward tension chain
A low monitor invites neck forward posture, which often recruits trunk bracing. Set your screen so your head can stay balanced over your torso. (Anecdote: when I finally raised my monitor by a few centimeters, I stopped doing that unconscious “turtle neck” that made standing feel like work.) If you’re working off a laptop, the easiest win is usually a stand + screen change—this guide on laptop stand vs external monitor helps you choose the least annoying upgrade.
Footrest strategy: alternate sides on purpose
Footrests aren’t just for seated ergonomics. In standing, they create a hip angle change—often soothing on nerve-sensitive days.
- Cycle: Left up 60–90 seconds → both feet 30 seconds → Right up 60–90 seconds
- Keep the footrest low enough that you’re not hiking a hip aggressively
Anti-fatigue mat rules: when it helps, when it irritates
Mats can reduce foot fatigue, but some people feel worse if a mat encourages them to stand longer than their current tolerance. If you get a mat, treat it like a tool—not a permission slip to statue-stand for an hour.
Shoes + support: the quiet variable most desks ignore
Hard soles and minimal support can increase lower-limb fatigue and encourage knee locking for “stability.” If you’re at home, experiment with different footwear (or supportive house shoes) and notice whether it changes how quickly symptoms ramp.
Show me the nerdy details
Ergonomic adjustments work best when they reduce the need for constant muscular co-contraction. Small changes in reach distance, monitor height, and foot support can reduce perceived threat to balance, which reduces bracing. A workstation that supports micro-movements (footrest cycling, slight weight shifts, brief walks) aligns with the idea that the body tolerates variability better than rigidity.
- Measure your standing elbow height (floor to elbow, relaxed shoulders)
- Measure screen center height relative to your eyes
- Note your symptom onset time when standing still
- Decide if you need a footrest, a perch stool, or both
- Write down your “non-negotiable”: no statue standing
Neutral action: Use measurements first; shop second. It prevents expensive mistakes that look ergonomic but feel awful.
Common mistakes: the “statue stance” and other flare triggers
Standing desks don’t hurt people. Static standing hurts people. And the most common mistake is thinking “good posture” means “hold still.”
Mistake #1: Standing perfectly still to “have good posture”
Stillness is the trap. If you want a single rule that actually works: movement beats correctness. The moment you catch yourself statue-standing, you’re already late—so reset kindly and move on.
Mistake #2: Squeezing glutes all day (over-bracing)
Some posture advice turns people into tightrope walkers. If your glutes are clenched while you read emails, your body is on high alert. That’s not stability; that’s over-protection.
Mistake #3: Forcing “ramrod straight” or flattening the low back
For many, “straight” becomes “rigid.” A little natural curve is not moral failure. Your spine isn’t a ruler. It’s a spring.
Let’s be honest… standing shouldn’t feel like punishment
If you dread your standing desk, your system has learned that standing equals danger. The fix is to rebuild trust with short, safe exposures and plenty of variability. (Anecdote: I had to make standing “easy again” by permitting myself to sit whenever symptoms started—not after they escalated.)
- Lock knees and hold still
- Clench glutes “for posture”
- Force a flattened low back
- Soft knees + 60/40 shifts
- Relaxed glutes; breathe
- Neutral spine + micro-movement
Sit vs stand vs lie down: choose by symptom pattern (not guilt)
This section is here because people punish themselves with “I should stand more.” No. You should choose the position that reduces symptoms and lets you work—today. Then you gradually rebuild tolerance. If you want a ready-to-use rhythm for desk days, use a sit-stand schedule for sciatica-friendly desk work instead of relying on mood.
If standing still hurts but walking helps: what it usually means
Often, you need movement and load variation. Try: short stand blocks + short walks + perch breaks. If walking helps, use it as your reset, not as a last resort.
If sitting worsens fast: adjust hips/knees/seat support first
Some people collapse into posterior pelvic tilt when sitting, loading the low back. If sitting worsens symptoms, try a slight perch (hips a bit higher than knees), support your low back gently, and keep feet grounded.
If nights are the worst: side/back positioning basics
If sleep is disrupted, consider gentle positioning changes (pillow between knees for side sleeping, or under knees for back sleeping). The goal is reducing twisting and excessive end-range positions. If night pain is escalating, that’s a “book soon” sign. If you need a simple starting point, see how to sleep with sciatica (especially the positioning basics).
When “unbearable” needs professional help (clear thresholds)
If pain is severe, worsening, or paired with neurologic symptoms, stop trying to win the day with grit. Get evaluated. The AMA has emphasized that numbness, weakness, or bowel/bladder issues should prompt earlier medical attention.
- Choose standing if soft knees + weight shift eases symptoms within 60 seconds
- Choose perch (half-sit) if standing still triggers symptoms but sitting feels okay
- Choose a short walk if walking reliably calms symptoms
- Choose rest + help if symptoms are severe, worsening, or neurologic red flags appear
Neutral action: Pick one option and run it for one work block. Reassess after.
Micro-breaks that work: 20 seconds, zero willpower
The best micro-break is the one you actually do. OSHA’s guidance for computer work emphasizes changing positions and moving periodically; that’s not wellness fluff—it’s basic mechanical reality. Your body wants variety. If you want the “why” plus a few no-drama routines, this pairs well with McGill Big 3 in 10 minutes—short, structured, and easy to dose.
The 20-second menu: ankles, hips, ribs—pick one
- Ankles: 10 heel lifts + 10 toe taps
- Hips: footrest swap (20 seconds per side)
- Ribs: 2 long exhales (4–6 seconds each)
- Steps: walk to the farthest room and back (yes, that counts)
The “two positions” plan: stand ↔ perch stool ↔ walk loop
If you have nerve sensitivity, “stand all morning” is rarely the winning strategy. Try cycles: 7 minutes stand → 7 minutes perch → 1 minute walk. Adjust the numbers to your onset time.
Timer script: what to label your reminder so it actually works
Don’t label it “stretch.” Label it something that matches your identity: “No-Statue Reset” or “Unlock + Shift”. (Anecdote: my reminders only started working when I stopped naming them like a self-improvement project and started naming them like a system.)
Here’s what no one tells you… the schedule beats the posture
You can have decent posture and still irritate symptoms if you don’t vary positions. Conversely, you can have “imperfect” posture and feel better if you move often. You’re not chasing elegance. You’re chasing tolerance.
- Pick a 20-second move you’ll actually do
- Cycle positions before symptoms ramp
- Rename reminders so they feel usable
Apply in 60 seconds: Set one reminder labeled “No-Statue Reset” for 25 minutes from now.
Short Story: The day I stopped “standing like a good person” (120–180 words) …
It happened on a normal Tuesday—the kind where you swear you’ll move more, then you don’t. I raised my desk, softened my knees (I thought), and got absorbed in writing. Ten minutes in, my leg started whispering. Twelve minutes in, it was shouting. I did the old routine: stretch hamstrings, brace harder, stand straighter—like I could bully my nervous system into cooperation. It got worse.
Finally, I sat down, exhaled slowly, and felt the tension drop like a curtain. The lesson wasn’t “never stand.” It was: I had turned standing into a test. So I rewrote the rules. Short stand blocks. Footrest cycling. Tiny ankle movement. A walk before the flare, not after. My desk stopped being a battleground. It became a station—one of several—and my body stopped treating it like a threat.

FAQ
Can a standing desk cause sciatica—or just reveal it?
A standing desk can aggravate symptoms if it increases static load, bracing, or knee locking. It may also reveal an existing sensitivity by changing how you distribute load during long work blocks. The goal is not “standing more,” but varying positions and keeping standing non-static.
Why does standing still trigger sciatic nerve pain?
Standing still can increase continuous muscle activation (calves/hips/trunk) and reduce circulation and variability. If your body responds by bracing and locking joints, tension can rise through the hip and low back region, making nerve-related symptoms more likely to flare.
Should your knees be locked when standing?
No—especially if you’re dealing with sciatica-like symptoms. Locking creates a rigid column and makes weight shifting harder. A micro-bend (not a squat) keeps the system adaptable and reduces end-range joint stress.
How long should I stand at a standing desk if I have sciatica?
Use your symptom onset time as your guide. If symptoms ramp at 12 minutes, don’t stand 12 minutes. Stand 7 (onset minus a buffer), then switch positions. Build tolerance gradually—think weeks, not hero days.
Is it better to sit or stand with sciatica?
It depends on your pattern. If sitting worsens quickly, adjust sitting mechanics (perch, lumbar support, feet grounded). If standing still worsens, shorten stand blocks and add movement/footrest cycling. If walking helps, use walking as your reset tool.
Do anti-fatigue mats help sciatica symptoms?
Sometimes. Mats can reduce foot discomfort, but they can also tempt you into longer static standing than your current tolerance allows. If you use a mat, pair it with scheduled micro-movement and short stand blocks.
Should I stretch hamstrings if standing triggers sciatica?
Be careful on flare days. If symptoms are nerve-sensitive, aggressive hamstring stretching may feel like “more pull” without relief. Try gentle motion, weight shifts, breathing-based de-bracing, and short walks first. If stretching helps, keep it mild and avoid pushing into symptoms.
Can shoes or insoles reduce sciatica while standing?
They can influence how your lower limb tolerates standing. If your feet fatigue quickly, you may lock knees for stability. Supportive footwear can reduce that tendency—but it’s not a substitute for movement and workstation setup.
When should I see a doctor for sciatica-like pain from standing?
Seek prompt care for weakness, foot drop, bowel/bladder changes, or rapidly worsening symptoms. Book evaluation if pain worsens over days, disrupts sleep, or doesn’t improve with conservative changes. Nerve-related symptoms deserve respect.
What’s the fastest way to calm sciatica pain at my desk?
Try the 60-second reset: soften knees, stack ribs over pelvis, shift 60/40, and add 10–15 seconds of ankle movement. If standing still remains provocative, switch to a perch or take a short walk. If symptoms keep recurring, a clinician-guided plan like physical therapy for sciatica can be a practical next step.
Conclusion: make the next 15 minutes count
Remember the curiosity loop from the beginning—why it waits until minute 12? Now you know: your body isn’t betraying you. It’s responding to static standing + locked knees + bracing like it’s a small, repetitive stress test. The fix isn’t dramatic. It’s systematic.
Here’s your 15-minute plan:
- Do the 60-second reset once.
- Set a timer for your new stand block (onset minus 5 minutes).
- Add one piece of relapse prevention: footrest cycling or a perch option.
(Anecdote: the first time I followed a plan like this, I felt almost annoyed—because it was so simple. But that’s the point. The nervous system likes simple, repeatable safety cues.)
- Soft knees prevents the rigid-column effect
- 60/40 shifting reduces static load
- Short cycles beat long “perfect” blocks
Apply in 60 seconds: Start one work block with a footrest cycle: 60 seconds left, 30 seconds both, 60 seconds right.
Last reviewed: 2026-01-16
